ICU Harbors Nastier Bugs, Study Finds
- Share via
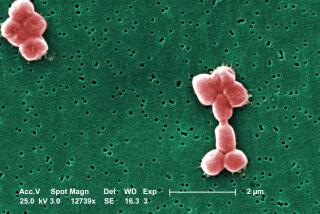
ATLANTA — Bacteria that can outsmart the drugs supposed to kill them are making intensive care units their breeding ground and giving patients infections they didn’t have when they checked in.
Excessive use of antibiotics and extremely ill patients--combined with an abundance of tubes--have made bacteria in the intensive care unit more resistant than those anywhere else in the hospital, according to a study by the Centers for Disease Control and Prevention and the Rollins School of Public Health at Emory University.
“The intensive care unit is the single most infectious place in the world when it comes to antibiotic-resistant bacteria,” said Dr. Alexander Tomasz of New York’s Rockefeller University, a drug-resistance expert.
Doctors long have thought that was the case, but they never had the evidence to tell them how bad the problem is. Now, armed with this study, researchers hope to find out which bugs plague each hospital the most so they can stop them.
“No one knows how to eradicate them,” said Dr. Lennox Archibald, a CDC medical epidemiologist and co-author of the study, which was published in the February issue of Clinical Infectious Diseases. “But we can reduce the chances of people getting sick.”
Antibiotics attack bacteria by demolishing part of their protective cell wall. To fight back, bugs can foil the antibiotic by changing the wall, so the medicines can no longer get in. They can also pass those new tricks on to other bacteria.
The study, conducted at eight hospitals in seven states from 1994 to 1995, compared the strength of common bacteria, such as staphylococcus and enterococcus, and the antibiotics commonly used to kill them. The hospitals were not identified.
Among the findings:
* 79.7% of staphylococcus epidermidis bacteria, which causes skin infections, was resistant to methicillin in ICUs--double the percentage of resistant staph found in other parts of the hospital.
* 39.4% of staphylococcus aureus, which causes blood infections and pneumonia, in intensive care units was resistant to methicillin, compared with 31.2% elsewhere in the hospital.
* 7.7% of enterococcus bacteria-- another cause of blood infections-- found in intensive care units was resistant to vancomycin, compared with 6.1% elsewhere in the hospital.
Bacteria can hide anywhere, and they can collect on clothing, blankets, walls and medical equipment. Hospital workers can pass them on by hand, and they can cling to tubes inserted into the body.
Intensive-care unit patients generally are the weakest, which puts them at even more risk for infection.
Drug resistance in hospitals means patients must take more expensive drugs and stay in the hospital longer. Some hospital-acquired infections can kill.
Drug resistance across the United States costs about $4 billion a year, the study says.
Stemming it may be a matter of going back to basics: washing hands, restricting antibiotic use and isolating the sickest patients.
“One of the most common ways bacteria are spread is through the hands of health care workers,” Archibald said. “I don’t care how good a doctor you are; at some point, you have forgotten to wash your hands.”
The study is an outgrowth of the CDC’s Hospital Infections Program, whose tracking system is the only national source of information on hospital-acquired infections.
“Each hospital is going to have to look at which of these organisms really represent a problem for them,” said Dr. John E. McGowan, an Emory professor of epidemiology and co-author of the study. “We are not going to have one uniform standard on how we deal with this.”
The study is a good start, said Richard Schwalbe, director of clinical microbiology labs at the University of Maryland at Baltimore.
“They looked at eight hospitals, which isn’t enough,” Schwalbe said. “It’s a good starting point, but this is a growing problem.”