A push to free more diabetics from daily shots
- Share via
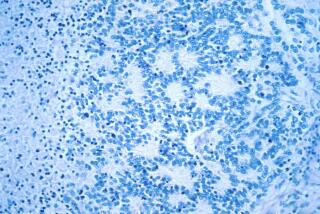
Hundreds of diabetics can now live without daily injections after receiving transplants of insulin-producing cells. These cells, taken from the pancreases of several cadavers, quickly set to work inside their new hosts to produce the glucose-regulating hormone.
But most diabetics aren’t candidates for the transplants. There simply aren’t enough organs available to provide the cells.
Two recent advances may eliminate this stumbling block, dramatically increasing the number of patients who can receive transplants of such cells. In one, the cells, known as islet cells, are taken from a live donor; in the other, islet cells are taken from just one cadaver.
“These cells can reverse diabetes,” says Dr. Bernhard J. Hering, director of the islet transplant program at the University of Minnesota in Minneapolis. “If we want to change the landscape of diabetes, we need an unlimited supply of islet tissue,” he said, and these two experimental techniques are significant steps in that direction.
Both would make daily insulin shots unnecessary.
Currently, such shots are a lifesaver for the nation’s 1 million people with Type 1 diabetes, whose islet cells are destroyed by their own immune system. (In Type 2 diabetes, the pancreas still produces some insulin.) Without insulin, the body can’t properly metabolize glucose, which it needs for fuel. As a result, toxic acids collect in the blood, and vital organs are starved of essential nutrients.
Even insulin injections and vigilant attention to blood sugar can’t match the islet cells’ continuous control over glucose levels. Almost all of the serious complications that result from diabetes, including nerve damage, blindness, kidney failure and heart disease, are caused by wide swings in blood sugar levels.
Although islet-cell transplants are an obvious solution, only 6,000 donor pancreases become available in the U.S. each year. Also, the fragile islet cells culled from cadaver organs can be severely damaged from cold storage or by the drugs given to recipients to prevent rejection; the pancreas itself can be damaged by poisons that circulate in the blood stream after brain death.
As a consequence, most islet transplants require two to four donor pancreases to produce enough cells for the recipient to become insulin independent.
In January, however, surgeons in Kyoto, Japan, successfully removed a portion of a healthy woman’s pancreas and extracted islet cells in the lab. The team then transplanted the insulin-producing cells into the woman’s daughter, who was severely diabetic.
The transplanted cells began producing insulin within minutes, and so far, the patient hasn’t required insulin shots. Her mother has remained healthy as well.
“The use of living donors will potentially allow us to treat many more desperate patients,” says Dr. James Shapiro, director of the islet cell transplant program at the University of Alberta in Edmonton, Canada, and a member of the Japanese surgical team.
The technique is still experimental, but doctors believe cells from healthy, live donors are better than ones from cadavers.
“We’re moving cautiously ahead,” says Shapiro. “While the risks of inducing diabetes in donors is very low, it would be a terrible tragedy if that happened, and their safety is paramount.”
Working on a parallel track, University of Minnesota researchers reported in February that they had devised a technique that uses cells from just a single cadaver pancreas. Scientists were able to limit the damage to cells when the pancreas was removed and the islets were extracted.
They also started recipients on immune-suppressing drugs before the patients were infused with the islet cells. A year later, all eight patients were insulin independent, and they had better glucose control than patients who had received islets from two to four donor pancreases.
“Maximizing the use of cadaver donors and making live donor transplants possible,” says Hering, “will give more patients better treatment choices.”
*
(BEGIN TEXT OF INFOBOX)
Advances in the insulin pump
Ultimately, mechanical devices may mimic the action of islet cells.
Within the next year, Medtronic MiniMed in Northridge plans to offer an external system that manages insulin around the clock. The device would combine an automated glucose sensor, which continually monitors blood sugar levels, with an insulin pump that releases the correct amount of insulin based on information from the sensor.
“This sensor-augmented pump will be the first big step toward the creation of a fully implanted artificial pancreas,” says Deanne McLaughlin, Medtronic’s communications manager.